In this article
Introduction to Protected Health Information (PHI): Safeguarding the Essence of Healthcare
In the vast landscape of healthcare, one term that takes center stage when it comes to data protection and patient privacy is PHI, or Protected Health Information. PHI is not just a collection of medical records; it’s the crux of healthcare data, encompassing a patient’s personal and medical information. This article delves deep into the world of PHI, exploring its significance, the scope of information it covers, the legal framework surrounding it, and the paramount importance of safeguarding it.
What is PHI?
Protected Health Information, or PHI, is a broad and encompassing term used in the healthcare industry to refer to individually identifiable information related to an individual’s medical history, health status, healthcare treatment, and payment for healthcare services. It is the very essence of a patient’s healthcare journey and includes a wide array of data points, from personal demographics to specific medical records. Let’s break down the key components of PHI to understand what it entails.
The Components of PHI
PHI encapsulates a diverse array of sensitive data that is not just integral to the healthcare process but also regulated by stringent laws, such as the Health Insurance Portability and Accountability Act (HIPAA). Understanding the components of PHI is not only essential for healthcare professionals but also crucial for ensuring the confidentiality, integrity, and availability of patient information.
This introduction serves as a gateway to exploring the multifaceted world of PHI, shedding light on the critical components that compose it and their significance in the context of patient care and data security. The intricate landscape of PHI allows us to comprehend how personal demographics, medical records, and insurance information, among other elements, weave the fabric of patient health data and why their protection is not just a legal obligation but a cornerstone of trustworthy healthcare services.
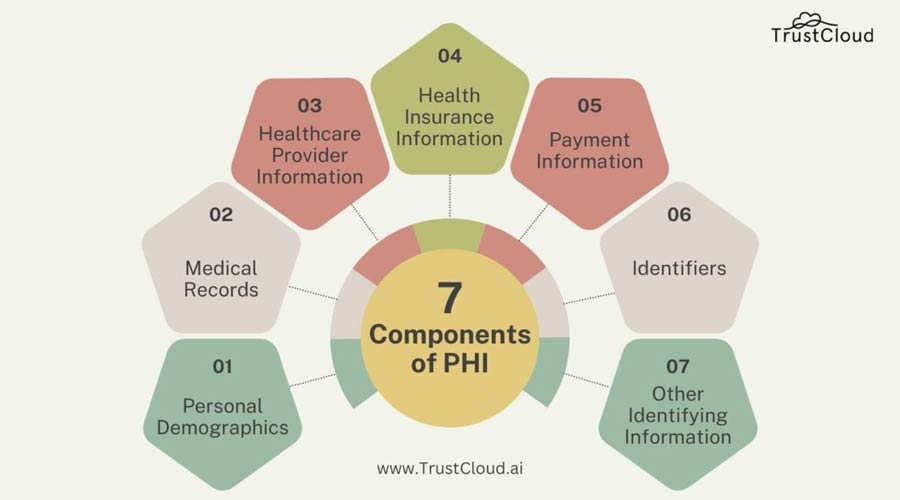
- Personal Demographics
At its core, PHI includes an individual’s personal information. This covers the basics, such as the patient’s name, address, date of birth, and contact details. These identifiers are crucial for distinguishing one patient from another and ensuring that their healthcare information is accurately attributed. - Medical Records
A significant portion of PHI revolves around an individual’s medical history and current health status. This encompasses a wealth of information, including diagnoses, treatment plans, medical test results, and details about past, present, or future medical conditions. Essentially, it’s the complete medical narrative of a patient’s life. - Healthcare Provider Information
PHI doesn’t stop at just the patient; it also extends to include information about healthcare professionals and organizations involved in the patient’s care. This could include data about doctors, nurses, hospitals, clinics, and any other entities responsible for delivering healthcare services. - Health Insurance Information
Given the pivotal role of health insurance in the healthcare ecosystem, PHI also includes information related to insurance policies, claims, and coverage. This information is essential for ensuring that healthcare providers receive proper compensation for their services. - Payment Information
The financial aspect of healthcare is intrinsically linked to PHI. Records of billing, payments, and insurance claims are all considered part of PHI. They provide a comprehensive view of how healthcare services are funded and delivered. - Identifiers
Unique identifying numbers, characteristics, or codes that distinguish one patient from another are also considered part of PHI. These identifiers are vital for accurate record-keeping and patient management. They could be patient ID numbers, social security numbers, or any other distinctive markers. - Other Identifying Information
PHI is all-encompassing, and it includes any information that could potentially be used to identify an individual. This could extend to photographs or any other characteristic that could distinguish one person from another.
The Legal Framework: HIPAA
The protection of PHI is not just a matter of ethics but a legal imperative. In the United States, the Health Insurance Portability and Accountability Act (HIPAA) serves as the bedrock of PHI protection. HIPAA is a comprehensive federal law that establishes strict guidelines for safeguarding the confidentiality, integrity, and availability of PHI.
Under HIPAA, healthcare providers, insurers, and other entities that handle PHI must adhere to rigorous privacy and security rules and protocols. These rules govern every aspect of PHI, from how it’s collected, used, and disclosed to the measures that must be in place to protect it.
Why is PHI protection so crucial?
In healthcare systems, the protection of Personal Health Information (PHI) stands as a paramount concern. This, encompassing sensitive details about an individual’s medical history, treatment, and payment records, holds a unique status in the realm of data security. The importance of safeguarding it extends far beyond mere compliance with regulations; it is fundamentally rooted in the trust between healthcare providers and patients, the sanctity of individual privacy, and the overall integrity of healthcare systems.
As technology evolves and the healthcare landscape becomes increasingly interconnected, the question of “Why is PHI protection so crucial?” is not only a matter of legal adherence but also a vital consideration for ensuring the well-being of individuals and the robustness of healthcare infrastructures worldwide. This exploration delves into the multifaceted reasons behind the imperative to protect it, examining the ethical, legal, and practical dimensions that underscore its critical significance in contemporary healthcare.
- Patient Privacy
At its core, PHI protection is about respecting and preserving patient privacy. Patients trust healthcare providers with their most intimate and personal information, and this trust forms the foundation of effective medical care. PHI protection is not just a matter of compliance; it’s a commitment to maintaining the sanctity of the patient-provider relationship. - Ethical Imperative
Beyond the legal requirements, there is an ethical imperative to safeguard PHI. Healthcare professionals are bound by a code of ethics that emphasizes patient welfare and confidentiality. Protecting it is an extension of this commitment to providing the best possible care to patients. - Legal Consequences
Non-compliance with PHI protection can have severe legal consequences. Violations of HIPAA regulations can result in hefty fines and even criminal charges. Furthermore, organizations that fail to protect it can face significant reputational damage, potentially eroding patient trust. - Trust and Reputation
In the healthcare industry, trust is everything. Patients need to feel confident that their information is secure and will not be mishandled or misused. Protecting it is not just a legal obligation but a cornerstone of maintaining the reputation and trustworthiness of healthcare organizations.
Access to PHI
Patients have rights when it comes to their PHI. Access to Protected Health Information (PHI) is a critical aspect of the Health Insurance Portability and Accountability Act (HIPAA), which prioritizes the privacy and security of individuals’ medical information. HIPAA grants patients the right to access their own PHI, allowing them to review and obtain copies of their health records held by healthcare providers, insurers, or other entities covered under HIPAA regulations.
This access empowers individuals to stay informed about their medical history, treatment plans, and test results, fostering transparency and involvement in their healthcare decisions. Healthcare providers are required to establish mechanisms that facilitate prompt and easy access to PHI, ensuring compliance with HIPAA guidelines while maintaining the confidentiality and integrity of sensitive health information.
Access to PHI under HIPAA not only promotes patients’ rights but also contributes to a more patient-centric and accountable healthcare system.
PHI in the Digital Age
In today’s digital age, the landscape of PHI has evolved. Electronic Health Records (EHRs) have become a standard practice in healthcare, transforming the way patient information is managed. EHRs offer several advantages, such as improved access to information and streamlined care coordination. However, they also present new challenges in terms of data security and privacy.
Ensuring the security of electronic PHI is of paramount importance. This involves implementing robust cybersecurity measures, access controls, and encryption to protect patient information from unauthorized access and data breaches.
Protected Health Information (PHI) is more than just a collection of medical records; it’s the lifeblood of healthcare data, encapsulating an individual’s personal and medical information. It represents the trust that patients place in healthcare providers and their commitment to preserving patient privacy.
PHI protection is not just a legal obligation but an ethical imperative and a critical aspect of maintaining the reputation and trustworthiness of healthcare organizations. In an era of digital transformation, the secure management of electronic PHI is paramount, ensuring that patient information remains confidential, secure, and accessible only to those with a legitimate need.
As we navigate the ever-evolving landscape of healthcare, PHI will continue to be the nucleus around which patient care revolves, and its protection will remain a cornerstone of the healthcare ecosystem.
Understanding the Risks Associated with PHI Breaches
The risks associated with PHI breaches can have severe consequences for individuals and organizations alike. When it is accessed or used without authorization, it can lead to identity theft, medical fraud, and financial loss. Additionally, breaches can result in reputational damage for healthcare providers, leading to a loss of trust from patients and the wider community.
Furthermore, the compromised integrity of it can have long-term implications for patients. When false information enters their medical records or when their health information is exposed to unauthorized parties, it can lead to misdiagnoses, improper treatments, or delays in receiving appropriate care. These risks highlight the importance of implementing robust security measures to protect PHI from breaches and unauthorized access.
Legal consequences of mishandling PHI
Mishandling PHI can have serious legal ramifications for healthcare organizations. Under HIPAA, the Office for Civil Rights (OCR) is responsible for enforcing the Privacy Rule and Security Rule, which govern the protection of PHI. The OCR has the authority to investigate complaints, conduct audits, and impose penalties for non-compliance.
The penalties for HIPAA violations can vary depending on the severity of the violation and the organization’s level of culpability. Violations can result in civil monetary penalties ranging from $100 to $50,000 per violation, with an annual maximum of $1.5 million. In cases involving willful neglect, penalties can be significantly higher, reaching up to $1.5 million per violation.
In addition to financial penalties, organizations that violate HIPAA may also face criminal charges. The Department of Justice (DOJ) can pursue criminal prosecutions for certain HIPAA violations, such as obtaining PHI for personal gain or with the intent to sell or use it for malicious purposes. Criminal penalties can include fines and imprisonment, depending on the severity of the offense.
It’s important to note that HIPAA violations not only carry legal consequences but can also result in reputational damage, loss of business, and erosion of patient trust. Healthcare organizations must take the necessary steps to prevent and mitigate the risks associated with mishandling PHI.
Best Practices for Protecting PHI
To ensure the protection of PHI, healthcare organizations and professionals must adopt best practices for safeguarding this sensitive information. Some key practices include:
- Access controls: Implementing strict access controls ensures that only authorized individuals can access PHI. This includes using strong passwords, multi-factor authentication, and regularly reviewing access privileges.
- Encryption: Encrypting PHI when it is stored or transmitted adds an extra layer of security. Encryption converts data into an unreadable format, protecting it from unauthorized access.
- Secure data storage: PHI should be stored in secure environments, whether it is in physical or electronic form. This includes using firewalls, antivirus software, and secure servers to prevent unauthorized access.
- Regular security audits: Conducting regular security audits helps identify vulnerabilities and weaknesses in the systems used to handle PHI. This allows organizations to take proactive measures to address any potential risks.
- Employee training and awareness: Healthcare professionals and employees should receive regular training on privacy and security practices. This ensures that they understand their responsibilities when handling PHI and are aware of potential risks and threats.
By adopting these best practices, healthcare organizations can significantly reduce the risk of PHI breaches and protect the confidentiality and integrity of patients’ health information.
Read more Compliance & Cybersecurity Articles from TrustCloud.
